Fortuna for
Health Plans
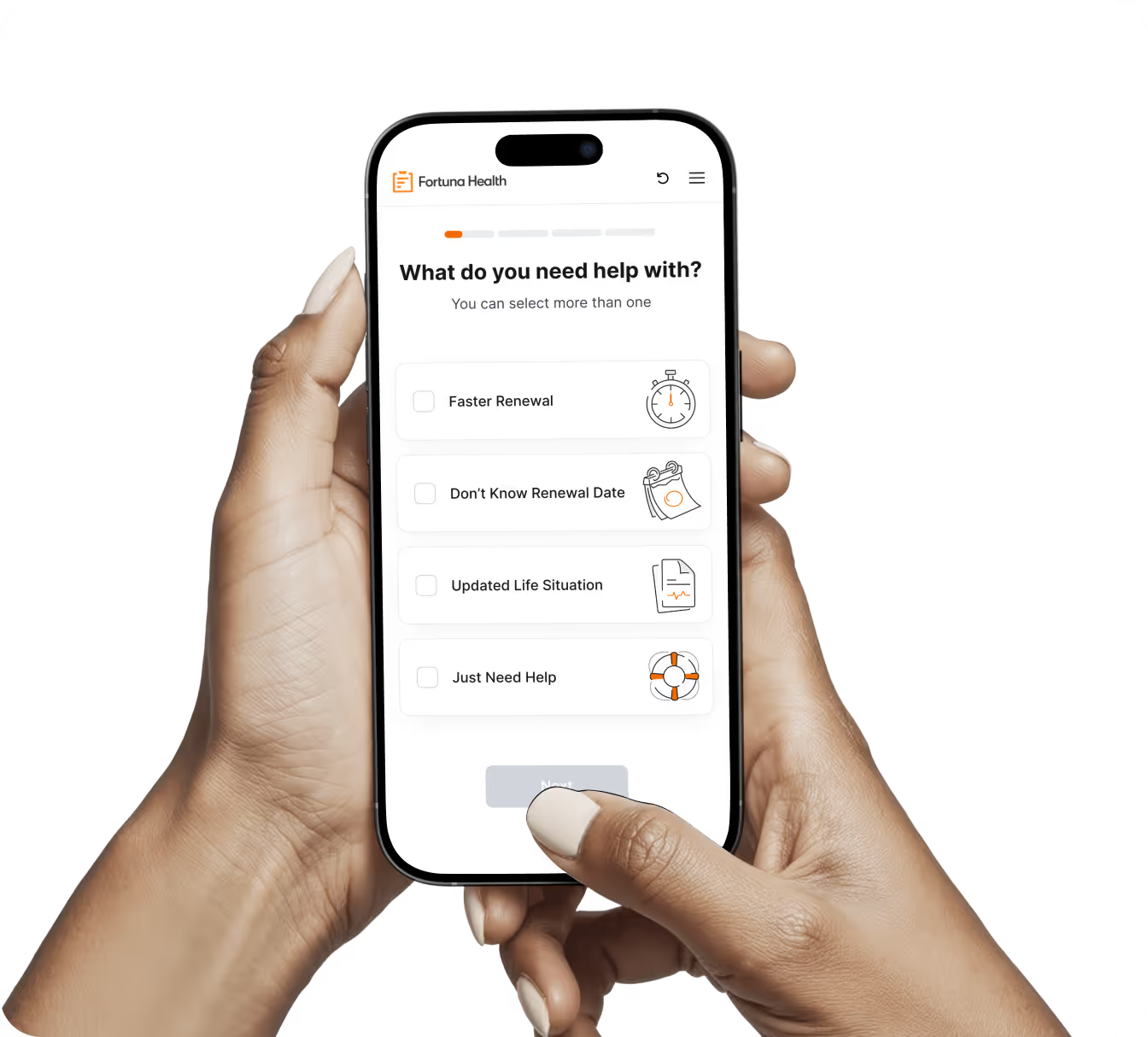
For your members, navigating Medicaid is always fast, simple, and digital with Fortuna.
Fortuna for
Health Plans
For your members, navigating Medicaid is always fast, simple, and digital with Fortuna.

Loved by members!
24/7 chat. Available in multiple languages. A trusted Medicaid navigator in your pocket.

My adult child has learning difficulties and is on the spectrum. I've known that I wanted to help my adult child apply for Medical Assistance ever since they turned 18-but I put it off. I got a Fortuna QR code from my clinic. I thought I'd give it a shot! IT WAS AWESOME. All done on my cell... 100% would recommend.

My mom’s Medicaid was about to lapse, but Fortuna stepped in just in time. Forever grateful.

FORTUNA TOOK THE CONFUSION OUT OF RENEWAL—SO SIMPLE AND FAST!! THANK YOU!
One Digital Platform
To Deliver You a Seamless Experience
languages over the phone




Renewal rate
languages over the phone




Unlock growth and retention
Become invaluable to your members by offering the easiest way to enroll and renew onto coverage. Let us handle all backend with states and counties.
Ongoing eligibility screenings
For simple and complex scenarios, always adding new state rules.
3rd-party integrations
For fast and secure application completion.
Real-time visibility
Into account statuses and incomplete steps.
SMS & email notifications
For action items like recert and document upload.
Guided navigation
With multi-lingual support by chat, SMS, and phone.
Consumer-first enrollment and renewal in one place
No more paper Medicaid forms, long call wait times, and lost recertification notices.
Ready to renew or start your coverage?
Take the next step and keep your Medicaid benefits active with Fortuna’s simple, guided process.








.avif)

.avif)